Sara started her day just like any other. She had been feeling nauseous early in the morning. Later, she felt tired and sluggish. “The workload is getting to me,” she thought.
As the day progressed, she felt worse and finally decided she must be coming down with a virus. Co-workers noticed that Sara was becoming irritable and confused. They suggested that she call her doctor.
When she went in to see her physician, he seemed very concerned. He ordered an EKG to be done in the office, then drew lab work. The physician then started asking questions about the history of heart disease in Sara’s family. “Why are you asking me about this?” Sara asked.
“I’m concerned you may have had a mild heart attack,” he responded.
“But that’s impossible. Women don’t have heart attacks!” she exclaimed.
Sara is one of many women who assume that heart disease affects mostly men. However, nearly 500,000 women die of heart attacks each year.
Symptoms for men usually include crushing pain in the chest, possibly radiating to the jaw or arm, shortness of breath and nausea. Women often do not present that typical picture, but have milder symptoms like Sara’s that are easily ignored and seen as just the effects of stress.
Women are likely to complain of fatigue, nausea, sometimes dizziness and confusion, shortness of breath and difficulty breathing, unexplained anxiety, weakness and cold sweats. The pain is likely to be in the abdominal region rather than the chest which further leads her to assume she is coming down with a virus, certainly not having a heart attack. What is even worse is the fact that women are almost twice as likely than men to die during the first year after a heart attack. Sara is fortunate. Her physician listened to her complaints and took her seriously.
Some women complain that their physicians do not seem to take them seriously and treat them as if they are just neurotic when they complain of vague symptoms. Chronic fatigue in women is commonplace, almost expected. Unfortunately, the lifestyle women live that requires constant rushing around and no time for self-care adds to the fatigue as well as the likelihood of developing heart disease.
But what exactly is heart disease?
Every time the heart beats, it sends oxygen-rich blood through the arteries to all parts of the body. Coronary artery disease develops as the blood vessels that lead back to the heart become clogged with plaque or with a fatty substance called cholesterol. As these build up in the vessel, more pressure is required to force the circulation of blood through them and the work of the heart muscle is increased. The arteries become stiff or hardened, a condition called atheroschlerosis, or more commonly, hardening of the arteries.
When the heart muscle cannot get the oxygen it needs because of the clogging in the vessels, one may experience pain called angina. Angina is actually a warning signal. If a woman is not checking her blood pressure or cholesterol to allow her early warning, she may have a heart attack before she is aware she has heart disease.
Damage to the cardiovascular system sets her up for congestive heart failure. When the heart muscle becomes damaged, it cannot effectively pump blood out and fluids collect in the lungs. Then she may experience weight gain of several pounds in a day, swelling of the hands, legs and feet and shortness of breath.
According to the American Heart Association in 1999, there were 17,346 deaths in Alabama related to heart disease. Of those deaths, 9,074 were women and 8,272 were men.
Women need to recognize that heart disease does affect them and to take measures to reduce their risk.
“Because heart disease does not start to affect women in the midlife period when men are first diagnosed, women often have the misguided perception that they do not have to worry about heart disease,” said Russell Reeves, a cardiologist with CardioVascular Associates P.C. in Birmingham. He added that actually, when heart disease hits women, usually 10 years later, “it hits with a vengeance.”
In the past it was believed that women develop heart disease about 10 years later than men do because the hormone estrogen was believed to protect women from heart disease. However, recent studies are raising questions about this belief.
Reeves stated that a recent study by the National Institutes of Health revealed that estrogen replacement therapy does little to reduce the risks of a second heart attack. It now appears that four to five years of therapy is required to reduce the risks for women who have already developed cardiovascular disease. Women are advised to talk with their physician about the benefits and risks associated with estrogen replacement therapy after menopause.
Estrogen may not be recommended if one has active liver disease, previous diagnosis of breast or uterine cancer, active gallbladder disease or a history of blood clots.
Caution is also advised for women who already have advanced coronary disease, chronic liver disease, diabetes, hypertension, are severely overweight or have a history of stroke.
Coronary heart disease is the number one killer in the United States with strokes being the number three and most debilitating type of heart disease. Strokes are sometimes referred to as a heart attack of the brain. The vessels in the brain become clogged or have spasms that interrupt the blood supply to a particular area of the brain.
Warning signs for strokes include: sudden confusion, difficulty speaking or understanding what is being said, sudden trouble seeing out of one or both eyes, numbness in one side of the face, numbness in the arm or leg of one side of the body, sudden trouble with balance, walking or coordination and sudden severe headache.
There are numerous factors that increase the risk of heart disease. A family history of heart disease or stroke increases the likelihood also. A person whose parent had a heart attack before the age of 65 or a sibling who had a heart attack before the age of 55, is at higher risk. It is also believed that African-American women are at greater risk than Caucasians. This may be associated with untreated high blood pressure.
Symptoms often neglected among many females
Related Posts

FDA, researchers seek methods of early detection of Alzheimer’s
October 1, 2024
A new blood test could help doctors diagnose Alzheimer’s disease more accurately in a primary care setting, leading to crucial
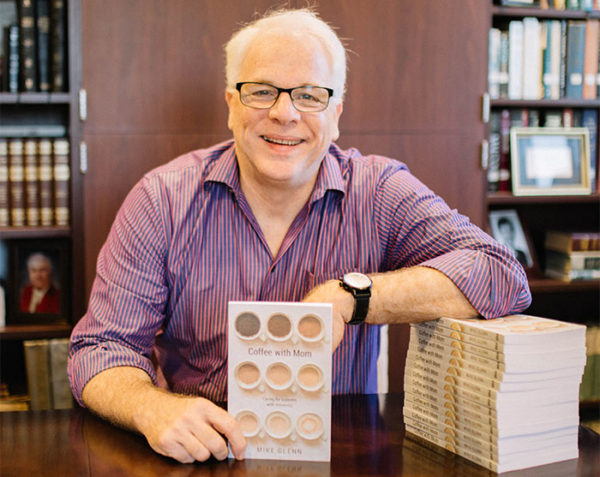
Alzheimer’s, dementia: Pastor shares lessons learned
August 12, 2019
As a minister for more than 40 years, Mike Glenn walked through the valley of dementia and Alzheimer’s disease with

Shame isolates, destroys community, psychiatrist says
October 13, 2016
Nobody needs a psychiatrist to explain what shame feels like — we all know, said Curt Thompson, a noted psychiatrist
Prenatal classes catalyst for new life, faith, churches
January 22, 2015
The young woman gingerly crawls off a motor scooter, grateful for the ride. Before, Kalliyan Seng could make the two-mile

Share with others: